Tissue Repair
The steps are
Types of wound healing
Healing by primary intention
Healing by secondary intention
Stages of repair
Stage of Hemostasis
Stage of inflammation
Stage of fibrosis
Brain
Heart
Nerves
General factor
Hypertrophic scar
- It is the process of healing after tissue injury.
- It begins as soon as the injury begins.
- It starts with the inflammation.
The steps are
- Stage of Hemostasis
- Stage of Inflammation
- Stage of Regeneration
- Stage of granulation tissue formation
- Stage of remodeling
Types of wound healing
Healing by primary intention
- Small wound
- Clean wound
- Minimal contamination
- The original tissue regenerates and heals
- Minimal to no scarring
- Functionally excellent
- Occurs in tissue with labile and stable cells.
Healing by secondary intention
- Large, gaping wound with tissue loss
- Infected wounds
- Wounds with the foreign bodies inside
- Heals with fibrosis
- Function is impaired because of scar contracture.
- Occurs in tissues with the permanent cells.
Stages of repair
Stage of Hemostasis
- Vasoconstriction
- Platelet aggregation
- Clot formation
Stage of inflammation
- Signs of inflammation
- Neutrophils recruit in the first 24 hrs
- Then they are replaced by macrophages after 3 days to week
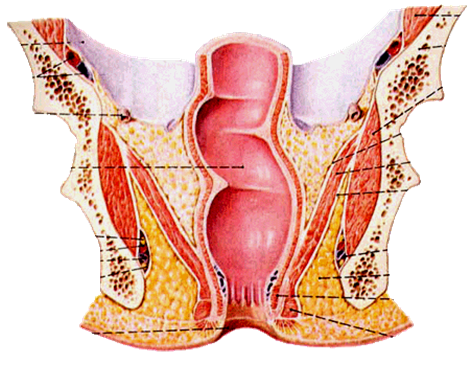
Stage of fibrosis
- The damaged tissue is replaced by granulation tissue
- It is mediated by different factors
- Cytokines by macrophages like IL1 and TNF
- Growth factors like TGF, VEGF, PDGF, EGF
- Granulation tissue has active fibroblasts and they are producing different ground substances
- There is angiogenesis
- Healthy granulation tissue looks pink in color with the serous discharge.
- The formed collagen is collagen type III in this phase.
Stage of remodeling
- The scar becomes smaller due to contraction
- It is mediated by myofibroblasts
- Excess tissue debris is collected by the phagocytes
- There is regeneration of the normal tissue if possible.
- It takes months to years.
- Contracture of the scar causes functional anomalies.
Repair in specific organs
Liver- regeneration of hepatocytes
Brain
- Gliosis
- Hydrocephalous ex vacuo
Heart
- Fibrosis
Nerves
- Wallerian degeneration
- Nerve regeneration along the nerve sheath if the sheath is intact.
Factors effecting wound healing
Local factors- Infection
- Foreign body in the wound
- Wound shape and size
- Site in the body
General factor
- Built
- Nutrition
- Co-morbid conditions
- Rest and exercise
- Habits like smoking and alcohol
- Age
Hypertrophic scar
- Large scar
- Injury site
- Up to 6 months
- Excess fibroblast
- Stops after sometime, no Rx
- Type III then type I
Keloid
- Scar that is very large and growing
- May extend away from injury site
- More than six months
- Due to genetic predisposition
- Rx needed, steroid or radiotherapy
- Type III excess

































.png)