Inflammation
Types
Events
Vascular events
Cellular events
Chemical events
Cardinal signs of inflammation
Increased vascular permeability due to
Azurophilic grannules-
Secondary grannules-
They have
Neutrophils migration and defence
Steps
Defect in adhesion occurs in
Types:
How does neutrophil recognizes the bacteria? (opsonins)
Oxygen dependent-
Oxygen independent killing
Complement system
They have different functions,
They have the following function
Chronic inflammation
Causes
Lymphocytes
Eosinophills and basophills
Key mediators are
Necrotizing inflmmation
Granulomatous inflammation
- It is an immediate response to injury.
Types
- Acute
- Chronic
Events
Vascular events
- Increased vessel caliber and permeability
Cellular events
- Recruitment of different types of inflammatory cells
Chemical events
- Production of different inflammatory mediators in the site of inflammation
Cardinal signs of inflammation
- Redness Due to vasodilatation due to histamine
- Heat
- Swelling Due to increased vascular permeability in respone to different chemical mediators like histamine, prostaglandins etc.
- Pain Due to bradykinin and p substance.
- Loss of function
Hemodynamic changes
- Initial transient vasoconstriction
- Followed by massive vasodilation due to histamine, prostaglandins and bradykinin.
Increased vascular permeability due to
- Vasoactive amines like histamine and serotonin
- End product on kinin system like bradykinin
- Cytokines like LTB4
- Direct injury of the vascular endothelium
- It increases the blood flow to the region and help in exudation as well as neutrophil migration.
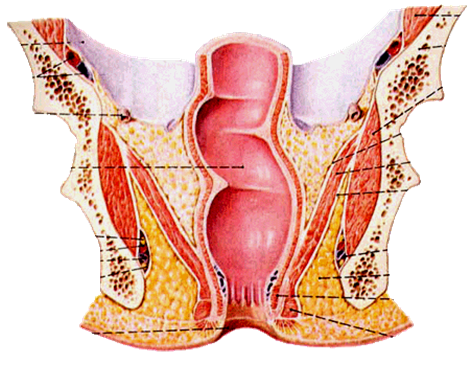
Cellular event
- The most important cellular event is the neutrophil migration.
- It is the commonest cell in the acute inflammation.
- It is also called as PMN.
- It has different grannules that carry the mediators of inflammation
Azurophilic grannules-
- that contains myeloperoxidase, phospholipase A2, lysozyme and acid hydrolase.
Secondary grannules-
- that contain lysozyme, phospholipase A2, leucocyte alkaline phosphatase etc
Macrophage
- It is after 48 to 72 hrs after the injury.
- They are large cell derived from monocyte that has lifespan for 2 to 4 months.
They have
- Elastase, acid hydrolases, and collagenases.
- Produce different cytokines like interleukins and TNF, that mediate inflammation and promotes the healing.
- They induce the production of different growth factors like FGF, EDGF, EGF and hence help in new tissue regeneration and repair.
- They engulf the debris that is remaining after the tissue is dead.
Neutrophils migration and defence
Steps
- Vasodilation and rolling
- Marginalisation
- Adhesion
- Diapedesis
- Chemotaxis
- Phagocytosis and degranulation
- Intracellular killing
- Adhesion is due to the surface molecules on the endothelium and the neutrophils like selectin and integrin respectively.
- These molecules are expressed due to other different chemicals like IL1, TNF etc.
Defect in adhesion occurs in
- DM
- Steroid therapy
- Uremia
- Alcohol intoxication
- Leukocyte adhesion defect (autosomal recessive cond.)
Chemotaxis
- It is the attraction of the inflammatory cells at the site of the tissue injury by the use of chemicals.
Types:
- Bacteria products like N-formyl methionine
- Inflammatory mediators like
- LTB4- product of arachidonic acid
- Complement proteins like C3a, C5a
- Chemokines like IL1 produced by macrophages.
Leucocyte migration
Phagocytosis
- It is the process of engulf the bacteria by neutrophils
How does neutrophil recognizes the bacteria? (opsonins)
- Coated by antibody
- Coated by complement C3b
- Plasma proteins like collectins
- The engulfed bacteria or product is called phagosome and when it combines with the lysosomes, it becomes phagolysosomes.
Intracellular killing
TypesOxygen dependent-
- Using superoxide radicals with the use of NADPH oxidase and producing superoxide and superchloride ions.
Oxygen independent killing
- Using lysozyme, lactoferrin, acid hydrolases which make pore in the bacterial cell wall and then causing the lysis of the bacteria.
- NADPH oxidase deficiency leads to the disease called as chronic granulomatous disease.
Chemical mediators of inflammation
Mediators of inflammation
- They are a group of proteins that are produced by the liver
They have different functions,
- C3a, C5a- chemotaxis and anaphylotoxins
- C3b- works as opsonin so it is target for phagocytosis and intra or extracellular killing
- C5b-C9- they form membrane attack complex.
TNF and IL
- They are produced by activated macrophages
They have the following function
- Fever
- Apoptosis
- Decrease apetite and cachexia
- Insomnia
- Stimulate the production of the different growth factors like EDGF, FGF, TGF etc.
- IL 8 is a chemoattractant.
Outcomes of inflammation
- Complete resolution with regeneration
- Complete recovery with scarring
- Chronic inflammation
- Abscess formation
Chronic inflammation
Causes
- Acute inflammation
- Persistent infections like TB
- Autoimmune disease
- Foreign body inside body
- Malignancy
Key players in the chronic inflammation
Macrophage - Modified macrophage is called epithelioid cell.
- Fused multiple macrophages makes giant cell.
Lymphocytes
- Types, B cell and T cell.
- B cell produce antibodies and T cells help B cells and also help cell mediated immunity.
Eosinophills and basophills
- mainly in the allergic conditions and worm infestations.
- Eosinophils has a protein in the cytoplasm called as major basic protein, that is toxic to the parasites.
Granulomatous inflammation
- It is special type of inflammation in which the infecting organisms living or dead are surrounded by macrophages(epithelioid cell and giant cell) and lymphocytes Th1, as well as plasma cells.
Key mediators are
- IFN gamma
- TNF alfa
- IL 2
- All are produced by activated T cells and macrophages.
- They convert the macrophages to epithelioid cells and giant cells.
- Common example is TB. If someone is taking TNF inhibitor like in RA like Infliximab and Etarnacept , they should do PPD test, otherwise they reactivate the latent TB.
Histologic patterns/types of inflammation
Exudative inflammation- Vascular permeability increases causing fluid and protein leak out of the blood vessel.
- Eg. Pneumonia, meningitis
Necrotizing inflmmation
- When inflammation causes an extensive tissue damage.
- E.g. Forunier gangrene caused by gram negative bacteria.
Granulomatous inflammation
- Slow growing organism like TB, fungi etc
Interstitial inflammation
- Like in the glomerulonephritis.
- Recruitment of the inflammatory cells in the interstitium.
Cytopathic inflammation
- When the infected cell in the tissue is altered.
- Mainly in viral infection like CMV inclusion bodies, Negri bodies in the rabies.
No inflammation despite infection
- Immunocompromised state like AIDS, steroids therapy, organ transplant receiver etc.




























.png)