Pelvis
Composition:
Two portions
Parietal pelvic fascia
Internal iliac artery
The relations are:
Internal iliac vein
External iliac lymph nodes
Common iliac lymph node
Position:
Sacral sympathetic trunk
Posteriorly
Laterally
Vessels and lymphatics of rectum
Arteries
Perineum
General features
Two triangles
An imaginary line drawn between the two ischial tuberosities divides perineum into anterior and posterior triangles
Anteriorly- it is continuous with:
Deep fascia has two layers
Superficial perineal pouch
Boundaries
Contents
Contents
Attached laterally to ischiopubic rami and ischial tuberosities
Formed by sphincter of urethra, deep transverse perineal muscle, superior and inferior fascia of urogenital diaphragm
Urinary structures
Ureter:
Course:
When empty, it is pear shaped with the following parts:
Relations:
Base/posterior-
Neck-
Superior-
Urethra
It is the organ for the external drainage of the urine.
It has dual function in males:
Parts:
Location:
It has two curves:
Relations
Peritoneum:
Anterior:
Posterior:
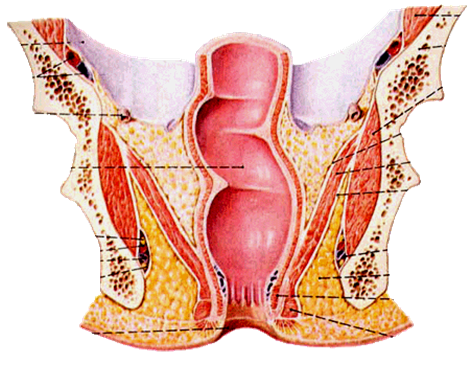
Anal sphincters
Internal
External
Ovaries
The boundaries of the ovarian fossa are:
relations:
Histology:
Blood supply:
Nerves-
Uterine tubes:
Location:
Parts:
Blood supply-
Lymphatics:
Uterus
Position:
Supports of the uterus:
They are:
Primary support:
Mechanical support:
Secondary supports:
Histology:
Parts:
Vagina:
Walls:
Fornices
Nerve:
Composition:
- formed by paired hip bones, sacrum, coccyx, and their articulations
Two portions
- Greater pelvis
- Lesser pelvis
- Terminal line ( pelvic inlet): formed by promontory of sacrum, arcuate line, pectin of pubis, pubic tubercle, upper border of pubic symphysis
- Pelvic outlet: formed by tip of coccyx, sacrotuberous ligament, ischial tuberosity, ramus of ischium, inferior ramus of pubic symphysis
Muscles of pelvic wall
- Piriform m.
- Obturator internus m.
Muscles of floor of pelvis
Levator ani
- Levateo prostate (pubovaginalis)
- Puborectalis
- Pubococcygeus and iliococcygeus
- Coccygeus
Pelvic diaphragm
- Superior fascia of pelvic diaphragm
- Levator ani
- Coccygeus
- Inferior fascia of pelvic diaphragm
Pelvic fascia
- A continuation of the transverse fascia into the pelvis. It coves the piriformis and obturator internus
- Attaches to the arcuate line of the pubis and ilium, thickens over the obturator internus to form the arcus tendineus, the origin of portions of the levator ani muscle
- At the tendinous arch of levator ani it splits to cove both superior and inferior surfaces of the levator ani as superior and inferior fascia of pelvic diaphragm
Visceral pelvic fascia
- Lies between the peritoneum and the pelvic viscera
- It is a continuation of the extra peritoneal connective tissue
- Ensheathes retroperitoneal viscera and forms septa between retroperitoneal organs
- Rectovesical septum
- Rectovaginal septum
Retropubic space
- Lies between pubic symphysis and urinary bladder
Pararectal space
- Lies around the rectus
Retrorectal space
Common iliac artery
- Continuation of abdominal aorta at level of L4 vertebra
- Terminates in front of sacroiliac joint by dividing into internal and external iliac arteries
Internal iliac artery
- It is a terminal small branch of the common iliac artery.
- It is about 4 cm long.
- In the foetus, this artery is the origin of the umbilical arteries to the placenta.
- It begins in front of the sacroiliac joint, between L5 and sacrum, medial to psoas muscle, and runs backwards and ends near greater sciatic notch by dividing in to two branches, the anterior and the posterior division.
The relations are:
- Anterior- ureter
- Posterior- internal iliac vein
- Lateral- external iliac vein and the obturator nerve
- Medial- peritoneum and the tributaries of the internal iliac vein.
Anterior division
- Superior vesicle artery
- Obturator artery
- Middle rectal artery
- Inferior vesicle artery
- Inferior gluteal artery
- Internal pudendal artery
- Vaginal artery
- Uterine artery
Posterior division
- Illiolumbar artery
- Lateral sacral artery
- Superior gluteal artery
Uterine Artery
- about 2cm from neck of uterus it crosses above and in front of ureter
Internal pudendal artery
- Perineal artery
- Anal artery
- Dorsal artery of penis (clitoris)
Veins of pelvis
- Parietal tributaries: accompany with arteries
- Visceral tributaries
- →superior rectal vein→inferior mesenteric v.
- ①Rectal venous plexus →inferior rectal vein→internal iliac v.
- →anal vein→internal pudendal v.
- ②Vesical venous plexus →vesical v.
- ③Uterine venous plexus →uterine v.
- External iliac– accompany the artery
- Common iliac vein– formed by union of internal and external iliac veins in front of sacroiliac joint, end upon L4~L5 by uniting each other to form inferior vena cava
The lymphatic drainage of pelvis
Internal iliac lymph node- Surround internal iliac vessels
- Receive afferents from pelvic viscera, perineum, buttock and back of thigh
External iliac lymph nodes
- Lie along external iliac artery
- Receive afferents from lower limb and some parts of pelvic viscera
- Sacral lymph node
Common iliac lymph node
- Lie along common iliac artery
- Receive afferents from all the above nodes
- Efferents pass to lumbar lymph node
Sacral plexus
Formation:- formed by anterior rami of L4 and L5 spinal nerves (the lumbrosacral trunk) and anterior rami of sacral and coccygeal nerves
Position:
- lies in pelvic cavity, anterior to sacrum and piriformis
Branches
- Superior gluteal
- Inferior gluteal
- Pudendal
- Posterior femoral cutaneou
- Common Sciatic
- Autonomic plexuses of plevic
- Hypogastric plexus
- Superior hypogastric plexus : lies in front of L5 between common iliac ateries
- Inferior hypogastric plexus (pelvic plexus): lie on each side of rectum
Sacral sympathetic trunk
- Is continuos above with the abdominal part
- Has 4or 5 ganglion
Relationships of rectus
Anteriorly- In male
- Fundus of bladder
- Seminal vesicle
- Prostate
- Ampulla ductus deferentis
- In female
- neck of uterus
- Vagina
Posteriorly
- Sacrum and coccyx
- Piriformis
- Median sacral vessels
- Anterior branches of sacral and coccygeal nerves
- Sacral sympathetic trunk
Laterally
- Pelvic plexus
- Superior and inferior rectal vessels
- Levator ani
Vessels and lymphatics of rectum
Arteries
- Superior rectal a.
- Inferior rectal a.
- Median sacral a.
- Lymphatic drainge Lymphatics follow arterial blood supply to following nodes:
- Superior rectal ln.
- Inferior mesenteric ln.
- Pararectal ln.
- Internal iliac ln.
- Sacral ln.
Perineum
General features
- Region of below pelvic diaphragm
- A diamond-shape space whose boundaries are those of the pelvic outlet
- Lower border of symphysis pubis
- Rami of pubis and ischium
- Ischial tuberosities
- Sacrotuberous ligament
- The coccyx
Two triangles
An imaginary line drawn between the two ischial tuberosities divides perineum into anterior and posterior triangles
- Urogenital region (anterior)-differs in male and female
- It has urogenital diaphram, which is made by,
- Muscles- sphincter urethrae and deep transverse perinei
- Fascia- superficial and deep urogenital fascia
- Anal region (posterior)-similar in both sexes
Branches
- Superior gluteal
- Inferior gluteal
- Pudendal
- Posterior femoral cutaneou
- Sciatic Common
Urogenital region
Superficial fascia has two layers- The superficial or fatty layer
- The deep or membranous layer (superficial fascia of perineum or Colles fascia)
Anteriorly- it is continuous with:
- Dartos of the scrotum
- Fascia of the penis
- Membranous layer of superficial fascia of the abdominal wall known as the fascia of Scarpa
Deep fascia has two layers
- Superior fascia of urogenital diaphragm
- Inferior fascia of urogenital diaphragm
Superficial perineal pouch
Boundaries
- Lies between inferior fascia of urogenital diaphragm and superficial fascia of perineum
- Space open anteriorly (In rupture of cavernous part of urethra, urine can extravasate from scrotum upward in front of symphysis pubis into anterior abdominal wall deep to membranous fascia of Scarpa)
Contents
- Posterior part-superficial transverse perineal muscle
- Lateral part-crus penis (male), crus of clitoris (female) and ischiocavernousus covering them
- Central part-bulb of urethra (male), bulb of vestibule (female) and bulbocavernousus covering them
- Branches of pudendal nerves and internal pudendal vessels
Deep perineal space
Lies between superior and inferior fascia of urogenital diaphragmContents
- Deep transverse perineal muscle
- Bulbourethral gland (male)
- Sphincter of urethra (male),urethrovaginal sphincter
- Ateries, veins and nerves
Urogenital diaphragm
Triangular in shapeAttached laterally to ischiopubic rami and ischial tuberosities
Formed by sphincter of urethra, deep transverse perineal muscle, superior and inferior fascia of urogenital diaphragm
perineal body
- Wedge-shape fibromuscular mass
- In female, between anal canal and lower end of vagina,
- In male, between anal canal and root of penis
- It is larger in the female than in the male and five support to the posterior wall of the vagina
Origin or insertion of several small muscles and insertion of part of palvic diaphragm
These muscles are:
- Sphincter ani externus
- Levator ani
- Superficial transverse muscle perineum
- Deep transverse muscles perineum
- Bulbocavernousus
- Sphincter of urethra (male) or urethrovaginal sphincter (female)
Pelvic organs
- Male reproductive organs
- Female reproductive organs
- GI organs like rectum and anal canal
- Urinary system organs like distal ureter, bladder and the urethra.
Urinary structures
Ureter:
- They are narrow paired tubes that convey the urine to the bladder.
- 25 cm long and 3mm in diameter.
- Upper half is in the abdomen and the lower half in the pelvis.
Course:
- Begins from the renal pelvis.
- Passes downwards and slightly medial to the psoas muscle.
- Crosses the external iliac artery near its origin from the common iliac artery to reach the pelvis.
- Runs along the greater sciatic notch, medially and posterior.
- Then comes anterior and medially to reach the base of the bladder.
Constrictions:
- At pelviureteral junction
- At when it passes into the pelvis, crossing the internal iliac artery
- At its insertion into the bladder, called as vesicoureteral junction.
Blood supply:
- Upper part- renal artery
- Middle part- branches of the aorta
- Inferior part- branches from the vesicular, middle rectal and uterine vessels.
Nerve-
- smpathetic and parasympathetic from the T10-L1 and S2-4 respectively.
It has an important relation with the uterine artery in its forward course, it passes beneath the uterine artery in the extraperitoneal sheath between the medial and the lower part of the broad ligament. Here it can be ligated or cut during the hysterectomy.
Urinary bladder
- It is the site of temporary storage of urine.
- The size, location and shape depends on the amount of the urine that the bladder contains.
- It is in the pelvis when empty, but comes to the abdomen when its full.
When empty, it is pear shaped with the following parts:
- Apex forward
- Base backwards
- Neck below attached with the urethra and
- Three surfaces- superior, right and left inferolateral
Relations:
- Anterior: apex is connected to the umbilical by median umbilical ligament (degenerated urachus).
Base/posterior-
- cervix and vagina in females
- males- rectum superiorly by rectovesical pouch, and inferiorly fascia of denonvillers with the seminal vesicles and the vas deferens.
Neck-
- Males- related to the prostate gland.
- Female- it lies in the pelvic fascia.
Superior-
- its covered by the peritoneum.
It is the organ for the external drainage of the urine.
It has dual function in males:
- Ejaculation
- Urine voiding.
- But is has only the urinary function in the female.
- The length is 15-20 cm in the males, and it is only 4 cm in females.
- Blood is supplied by the branches from the prostatic vessels and the penile vessels.
Parts:
- Prostatic part (3cm)- beneath the prostate gland
- Membranous part(2cm)- inside the pelvic diaphragm
- Spongy or penile part(15 cm)- inside the corpus spongiosum in the penis, ventral surface.
- The prostatic urethra is only the homologus part of the female urethra.
The opening of the urethra is guarded by two sets of sphincters:
Internal sphincters
- they are just the condensation of the muscles of the bladder in circular fashion around the neck of the bladder.
- They are supplied by the autonomic fibers.
- They are functional in man, and less in woman.
- Their function is the control of the retrograde ejaculation, no the urine continence.
External sphincter:
- Located in the urogenital diaphragm.
- Has circular muscles, called as sphincter urethrae.
- It is supplied by pudendal nerve.
- It is under voluntary control.
- They are developed in both males and the females.
- Function is the urinary continence.
Lymphatic drainage:
- from the prostatic and membranous part is to the internal iliac nodes, and
- from the penile part is to the deep inguinal nodes.
Rectum
- It lies between the sigmoid colon and the anal canal.
- When it is full, person will have urge to defecate.
Location:
- In the true pelvis, in front of the S3-S5.
- Length is 12 cm and is 4 cm wide.
It has two curves:
- anteroposterior- first anterior, then posterior.
- Lateral- first convex to right, then left and then again right.
Relations
Peritoneum:
- Upper third- covered by peritoneum from the sides and the front
- Middle 3rd- only front
- Distal 3rd- no peritoneum.
Anterior:
- Males- rectovesical pouch with intestines, urinary bladder, seminal vesicle and prostate from up to down.
- Females- rectouterine pouch, cervix and vagina.
Posterior:
- Sacrum
- Pyriformis
- Sacral vessels
- Sympathetic chain and nerves.
It has three prominent mucosal folds, called as the valve of Heuston, the function of these valves is not clear.
They are also called as plica transversalis.
Blood supply:
- Superior rectal artery- (main artery) branch of the inferior mesenteric artery
- Middle rectal – branch of the internal illiac
- inferior rectal artery- branch of internal pudendal artery.
- Median sacral- arises from the back of aorta.
Venous drainage
- Superior rectal vein- goes to Inf. Mes. Vein (portal)
- Middle and Inferior rectal vein- to internal iliac vein (systemic)
Lymphatics
- Superior half- to the inferior mesenteric nodes
- Inferior half- internal iliac nodes.
Anal region
Internal
- Smooth muscle (thickened circular muscle coat)
- Surrounds upper two-thirds of anal canal
- Autonomic nerve supply
External
- Striated muscle
- Surrounds lower two-thirds of anal canal
- Three parts-subcutaneous, superficial and deep
- Innervation by anal nerves of pudendal nerve and branches of S4
Inner surface:
- Inner surface is divided into upper 15 mm and below 25 mm by a line called as pectinate line.
- The upper part is developed from the anorectal membrane (part of cloaca, and the inferior is from the invagination of the ectoderm).
- The upper part has mucosal folds called as the folds of Morgagni.
Sphincters-
- There are two sets of sphincters,
- External sphincters
- Internal sphincters.
- The internal sphincters are made of the condensed circular muscles of the wall of the anal canal, that covers the proximal 2 cm of the length of the wall of the anal canal. It is involuntary.
- The external sphincter is striated, and is voluntary. It covers all the length of the anal canal. It has three parts, sub-cutaneus, superficial and deep parts.
Blood supply:
- Arterial supply
- Above the pectinate line- sup. Rectal artery
- Below the pectinate line- inf rectal artery
Venous drainage:
- Superficial and deep venous plexus, that drains into superior and inferior rectal veins respectively. There is free communication between these two channels, and is a site of portocaval shunt.
- The internal venous plexus has the beginning of major veins in 3, 7 and 11 o’clock, the hemorrhoidal veins.
- Enlarged veins due to straining, tumors, or increased portal pressure is called varices, which can cause significant bleeding during defecation.
Lymphatics:
- Above pectinate line- to internal iliac nodes
- Below the pectinate line- to superficial inguinal nodes.
Nerve supply:
- Above pectinate line- autonomic nervous system
- Below pectinate line- somatic nerve, inferior rectal nerve (S2-S4)
Ischiorectal fossa
Paired, wedge-shaped, fat-filled spaces on either side of anal canal
Boundaries- Apex-conjunctive area of inferior fascia of pelvic diaphragm and fascia covering the obturator internus
- Base-skin of anal region
- Medial-sphincter ani externus, levator ani, coccygeus and inferior fascia of pelvic diaphragm
- Lateral-ischial tuberosity, obturator internus and fascia
Contents
- Fat
- Internal pudendal artery and vein and their rectal branches
- Pudendal nerve and its inferior rectal branch
Vessels and nerves enter from gluteal region, through lesser sciatic
foramen, travel on a fascial canal-the pudental canal (Alcock’s)
-on the lateral wall of fossa, and extend forward into urogenital region
Female reproductive organs
- Ovaries
- Fallopian tubes
- Uterus
- Vagina
- Vulva
Ovaries
- They are the female gonads.
- They lie on the fossa on the lateral pelvic wall, that is called as ovarian fossa.
The boundaries of the ovarian fossa are:
- Anterior- oblitrrated umbilical artery
- Posterior- ureter and internal iliac artery
relations:
- It is entirely covered with the peritoneum.
- It is connected to the posterior layer of the broad ligament by folds of the peritoneum, called as mesovarium, which contains the ovarian artery.
- The lateral part of the broad ligament that transmit the vessels of the ovary is called as the infundibulopelvic ligament.
- Development- from the gonadal ridge on th eposterior abdominal wall.
Histology:
- Cortex with the supporting and germ cells at different stages of development
- Medulla with the ground tissue, blood vessels and the lymphatics
Blood supply:
- Ovarian artery- branch of the abdominal aorta
- Vein- ovarian vein, right to IVC and left to renal vein.
Nerves-
- Sympathetic and parasympathetic nerves.
Uterine tubes:
- Development- from the paramesonephric (Mullerian) ducts.
- Also calles as fallopian tubes.
- 10 cm long.
Location:
- Free upper margin of the broad ligament.
Parts:
- Interstitial part- inside the wall of the myometrium
- Isthmus- narrow constricted part between the interstitial and the ampulla.
- Ampulla- dilated distal 2/3rd part
- Infundibulum with fimbria.
Blood supply-
- Medial 2/3rd by uterine artery
- Lateral 1/3rd by ovarian artery.
Lymphatics:
- Isthmus- to superficial inguinal nodes
- Rest all to aortic and preaortic lymph nodes.
Uterus
- It is called as womb.
- It lies in the true pelvis between the urinary bladder and the rectum.
- Pyriform in shape.
Position:
- Anteversion- the axis of the cervix makes an angle of the 90 deg with the long axis of the vagina, called as anteversion.
- Anteflexion- the long axis of the uterus makes an angle of 120 deg with the long axis of the cervix is called asteflexion.
- So the uterus lies anterior and superior to the vagina.
- If the uterus is lying posterior to the axis of the vagina, that’s called retroversion, that may predispose to miscarriage and uterine prolapse.
Supports of the uterus:
- The structure that provide stability to the uterus and prevent uterine descent.
They are:
Primary support:
- Pelvic diaphragm
- Urogenital diaphragm
- Perineal body.
Mechanical support:
- Uterine axis
- Pubocervical ligament
- Tranverse cervical ligament of Mackenrodt’s
- Uterosacral ligament
- Round ligaments of the uterus
Secondary supports:
- Broad ligaments
- Uterovesical fold of peritoneum
- Rectovaginal fold of peritoneus.
- Disruption of one or more of the herementioned structures, will cause uterine descent, called as the uterine prolapse.
Histology:
- Endometrium
- Myometrium
- Perimetrium
Parts:
- Cervix
- Body
- Fundus- posterior wall of the fundus is the commonest site of the implantation.
Vagina:
- Muscular organ
Walls:
- Anterior 6 cm
- Posterior 8 cm
Fornices
- Anterior
- posterior
- Lateral
- Mucosa- stratified squamos
- Blood- vaginal artery
- Lymphatics- internal iliac nodes
Nerve:
- Lower 3rd- pain sensitive and hence by pudendal nerve
- Upper 2/3rd by autonomic and hence are pain insensitive.
.png)
































No comments:
Post a Comment